Varicose Vein Treatment in the U.S. – Are CHIVA or ASVAL Practical?

When Insurance Stops Covering Varicose Veins, What About CHIVA or ASVAL?
Which is Better – CHIVA or ASVAL?
It’s like saying which is better: chocolate or vanilla?
It’s a personal preference. It’s not really based on hard facts or widely accepted rigorous double blinded controlled studies.
It’s really just what you prefer or feel.
The title’s questions also a beg a different kind of question which is the basis of this article.
What are the doctor’s priorities in treating varicose veins in the country in which they practice?
ASVAL vs. CHIVA is debated in Europe. In the United States, no vein specialists anywhere have an opinion – at all – or even cares.
Why?
The Answer is …
Phlebology American Style or …
Why is Phlebology All of a Sudden So Popular Amongst American Doctors?
Regrettably in the United States, health care eventually boils down to the money.
The bad news is that many of American vein doctors are more focused on which procedure makes them the most money.
Ablating the saphenous vein with laser or radiofrequency makes them thousands of dollars.
Saving the saphenous vein? – meh. Much less.
That’s an important reason why nobody at all in the U.S. cares about this controversy.
There are other reasons that we will discuss shortly.
Unlike many European colleagues who have incorporated phlebology in their training programs for over six decades, phlebology has never achieved the status of a totally recognized specialty in the U.S.
Phlebology in the United States is the bastard stepchild.
Unlike many of our European colleagues who have embraced phlebology for over six decades, phlebology has never achieved the status of a totally recognized specialty in the U.S.
Their indifference among American academics has resulted in the failure of teaching institutions to provide standardized training programs.
The financial support for such a board (which the American Board of Venous and Lymphatic Medicine wants so badly) supported by the necessary government funds is not a viable option. The Board of Vascular surgery will not allow a redundant standard training program which specializes in only veins to coexist.
Wannabe phlebologists in this country are left with trying to find experienced mentors, three-day conferences, or simply learning and at the same time practicing the vein procedure du jour as they go.
Consequently, their training and skill sets are unsystematic, chaotic, and inadequate.
Often new-fledged phlebologists in America are from questionable backgrounds or gravitate from other specialties after being burned out.
The ASVAL vs. CHIVA Debate
To answer the ASVAL vs. CHIVA debate, I need to briefly describe these two saphenous sparing techniques used to treat varicose veins.
Most vein specialists in the United States cannot describe or understand them. It takes some concerted effort.
Trying to understand these techniques – and their inevitable accompanying complex diagrams (especially CHIVA) – at a vein conference delivered by a European doctor speaking in their best English usually makes everyone’s eyes glaze over. My hat is off to them at the same time since like most Americans, I only speak one language.
French and Italian physicians have the most experience with these techniques. They seem to be captivated with the abundant convoluted permutations and the bewildering diagrams of the superficial venous pathophysiology of CHIVA.
European CHIVA advocates seem to feel that ASVAL is blasphemous. It’s contentious.
Explaining ASVAL and CHIVA clearly and quickly is no easy task.
To add to this challenge, I will refrain from using diagrams. (gulp)
It’s been said that most people have the attention span of goldfish. Research shows that the average blog post clicked off after eight seconds. If you’re still with me …
Here we go.
First, a disclaimer.
Neither of these techniques are very good for advanced varicose vein disease.
Especially ASVAL.
ASVAL for the Treatment of Varicose Veins
ASVAL is easier to understand and perform.
ASVAL stands for Ambulatory Selective Ablation of Varices under Local Anesthesia. It has been studied since 2009 and was pioneered by Paul Pittaluga.
It can be thought of simply as the elimination of the varicose vein tributaries by just performing extensive phlebectomies.
It assumes the ascending theory as the of cause of varicose veins. Traditionally, many U.S. physicians were taught that reflux starts in the saphenous vein and later extends into the tributaries which are the varicose veins visible on the surface of the skin. This is also known as the “waterfall effect”.
ASVAL advocates believe that you must catch the problem early before the “suction” from the varicose veins has secondarily and irreversibly and damaged the saphenous vein.
The saphenous vein valves can potentially eventually recover if the damage is not too bad or if it’s just segmental in nature. It’s better if valves of the sapheno-femoral junction are still normal.
In many early cases, the saphenous veins are entirely normal and only varicose veins are present. This is the reason that there is a growing tendency for insurance companies in the U.S. refuse to cover the treatment of varicose veins at this stage when they are often asymptomatic and cosmetic.
To perform ASVAL successfully, the vein specialist must deliberately reject patients with more advanced disease. Most varicose vein patients are classified as the earlier stage C2 disease and are treatable with ASVAL’s extensive phlebectomies.
If advanced skin changes or ulceration (C4 to C6 disease) have already occurred from the underlying venous disease, attempts at using ASVAL will result in a high rate of recurrence because the saphenous vein and its valves are already irreversibly damaged.
ASVAL proponents use other procedures like ablation and sclerotherapy only when the saphenous vein is not recoverable.
This technique is based on the concept that truncal venous incompetence is secondary to peripheral veins’ negative pressure causing a “sucking effect”.
The ascending theory is not 100% valid all of the time. In many vein specialist’s experience 10-20% (or more) of asymptomatic younger patients with spider veins have no varicose veins. They may have some degree of saphenous vein reflux even if it is segmental and does not involve the saphenous-femoral junction.
ASVAL criteria for best results include:
- Small saphenous vein preferably less than 6 mm in diameter.
- Younger patients who respond better.
- Women who have not had children also have superior results.
They also attempt to quantify the number of veins which have enlarged by numbering them. If 7 or less of the 32 possible described zones or areas of the leg contain varicose veins, the probability of a long-term success of saving the saphenous vein is 6.8 times increased and the chance of relieving symptoms was found to be 2.91 times increased.
In summary, since most varicose vein patients (especially women) present with mainly cosmetic concerns, ASVAL may be potentially very useful.
CHIVA for the Treatment of Varicose Veins
In practice, it is more difficult to perform CHIVA correctly compared with the less complicated ASVAL.
CHIVA is a French acronym for Conservatrice et Hémodynamique de l’Insuffisance Veineuse en Ambulatoire. It has been performed since 1988.
A classification with so-called abnormal hemodynamic “shunts” is the crux of the CHIVA approach. Proponents of this theory have illustrated four patterns of deviant flow in the superficial saphenous, varicose, and perforating veins.
Intervention requires simple ligation (thereby disconnecting the abnormal shunts) at either the saphenous vein junction or the origin of the varicose veins at the point where they come off the saphenous vein. Sometimes a combination of ligations is required. Normal flow then returns without destroying any veins at all. After the appropriate ligations, abnormal high-pressure veins are reportedly remodeled and return to their normal size.
After the strategic ligations are performed, normal flow from the superficial to the deep veins is reestablished. The blood flow is rerouted from an abnormal (deep to superficial) to a normal (superficial to deep) pattern.
No phlebectomies, sclerotherapy, or saphenous ablations are required!
To perform CHIVA, a detailed and exhaustive preoperative duplex ultrasound determines where and when the ligations are performed at critical reflux points.
Commonly the reflux points include the sapheno-femoral or sapheno-popliteal junction, the origin to the varicose vein tributaries or a combination of these.
Sometimes the ligations have to be delayed over six months for reentry perforators to develop from the saphenous vein to prevent thrombosis of the saphenous vein.
It’s the reentry perforators and their location that are critical to the success of classifying and subsequently correctly treating the incompetent veins. These reentry points are not usually mapped or noted by vascular technologists in the United states.
These critical reflux points are determined by a comprehensive and complicated scan.
Many vein specialists in our country rely entirely on their technologists to determine their course of action and don’t have the skills themselves to perform this test. It would be difficult for most vascular technologists to learn, perform and record this in extra information in addition to the present protocol.
It is extremely critical when performing this technique to identify all of the reentry perforators of the saphenous and/or varicose vein tributaries. They help determine which of the shunt scenarios exist. Once the shunt type is identified the appropriate vein ligations scan be performed.
CHIVA studies have been analyzed by Cochrane evidence based reviewers in 2013 and 2015. Overall bias across studies was said to be high because the lack of blinded studies. CHIVA was compared to stripping and in terms of recurrence and side effects was superior.
Only one study examined quality of life and favoring CHIVA over stripping. Quality of evidence was rated in the four randomized controlled studies due to the low to moderate because of the low number of events.
CHIVA method for the treatment of chronic venous insufficiency.” Cochrane Database Syst Rev. 2015;(6):CD009648.
Underlying Principals and Practicality of ASVAL and CHIVA
Two schools of thought exist, explaining the development and propagation of venous disease as an “ascending” and “descending” process, respectively.
The descending theory, stating that CVD is secondary to proximal disease (e.g. saphenofemoral/saphenous incompetence), is the most widely accepted when planning treatment aiming to remove or destroy the junction or truncal veins.
ASVAL assumes the ascending theory early in the disease process.
CHIVA doesn’t care which theory is correct.

That makes common use of the principles of CHIVA by the average vein practitioner untenable.
Duplex scanning of the superficial venous scanning is highly operator/technologist dependent.
Many vein doctors depend entirely on the vascular technician’s report to decide which procedures would best treat the underlying pathology.
Most doctors cannot perform a venous duplex scan themselves. Some doctors even need to utilize a technician to help perform ablation procedures and ultrasound guided sclerotherapy.
Acquisition of the duplex vascular ultrasound skills required for these procedures takes specialized extensive additional training, patience, and a high level of skill.
The CHIVA procedure demands an exceedingly complex and technically demanding duplex scan (including an unfamiliar Perthe’s exam which is currently not performed in the United States.)
It is imperative to look for a reentry perforating vein either from the saphenous vein or the varicose vein tributaries to first classify the different shunts and then properly treat that particular abnormal venous flow pattern.
In addition, for a Type 1 shunt, a high ligation of the great saphenous groin is required. For nonsurgeons, in an office setting especially in an obese patient, this will not be possible.
However, high ligation of the saphenous vein can be replaced by an endovenous ablation of only short a segment of the proximal great saphenous vein.
The closure success of only the proximal saphenous vein has never been studied but failure would inevitably be higher than ligation alone. Neovascularization, on the other hand, would be less than with the surgical/ligation option.
Conclusion
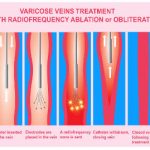
Most vein specialists in the world destroy an abnormal refluxing saphenous vein with laser, radiofrequency, sclerotherapy, stripping, or medical grade glue. This alone rarely produces happy patients.
Usually phlebectomy or sclerotherapy is required at some point to complete the treatment by removing the varicose vein tributaries.
This approach is in opposition to the ASVAL and CHIVA methods, whose principles are to preserve the saphenous vein as much as possible.
In ASVAL, the slightly refluxing saphenous is returned to normal or prevented from progressing to a more advanced stage by removing the varicose veins in the early stage. This is done by extensive phlebectomies alone.
CHIVA uses the abnormal saphenous and varicose veins as pathways to redirect flow back to normal after a series of ligations at critical points. Training programs are nonexistent in the U.S. Learning the technique is quite challenging, difficult to master, and remains a big obstacle.
Their preoperative duplex ultrasound requirements are impractical and overly burdensome. In the case of CHIVA, the learning curve is steep. It is difficult to master making it unfeasible for the average practitioner who depends on a sonographer who is not trained to perform the necessary venous duplex studies of this depth.
Randomized controlled trials to prove efficacy of ASVAL and CHIVA are difficult to perform since many of the patients come from private practice where financial support is not available.
Therefore, proof of efficacy of both saphenous sparing approaches is lacking.
The facts are that both received only class/level 2B recommendations from the American Venous Forum for CHIVA and similar 2B results from the European guidelines published in 2015 for ASVAL.
Therefore, CHIVA and ASVAL have not gained wide acceptance in the Unites States.
However, the financial advantage of ablating the saphenous vein is the real driver for not saving the saphenous vein in this country when treating varicose veins.
That’s ruthlessly honest.
Americans want their insurance to cover their varicose veins.
When that no longer happens, ASVAL and CHIVA may get another look.